You are looking at an archived version of our site. Please visit thepcc.org for a fresh, new experience!
You are here: Array » Improve Care in Medica ...
Improve Care in Medicare by Growing Primary Care in ACOs

Background
The Medicare Shared Savings Program (MSSP) is the oldest Medicare value-based payment model currently in operation, with more than 10 years of experience and related data. Authorized in 2010 in the Affordable Care Act, MSSP is not a temporary demonstration model. It is a voluntary program for providers, and beneficiaries are free to seek care from any provider participating in traditional Medicare.
Clinicians and other providers participate in MSSP by forming accountable care organizations (ACOs). ACOs sign agreements with CMS taking responsibility for quality and total cost outcomes for a specific population of beneficiaries attributed to the ACO’s participating primary care clinicians.
Both CMS and Congress have made changes to MSSP since its inception, yet two program results have remained constant:
- “Physician-led” ACOs generate greater savings on average when measured in percentage and per beneficiary terms.1
- ACO performance improves with duration in MSSP.
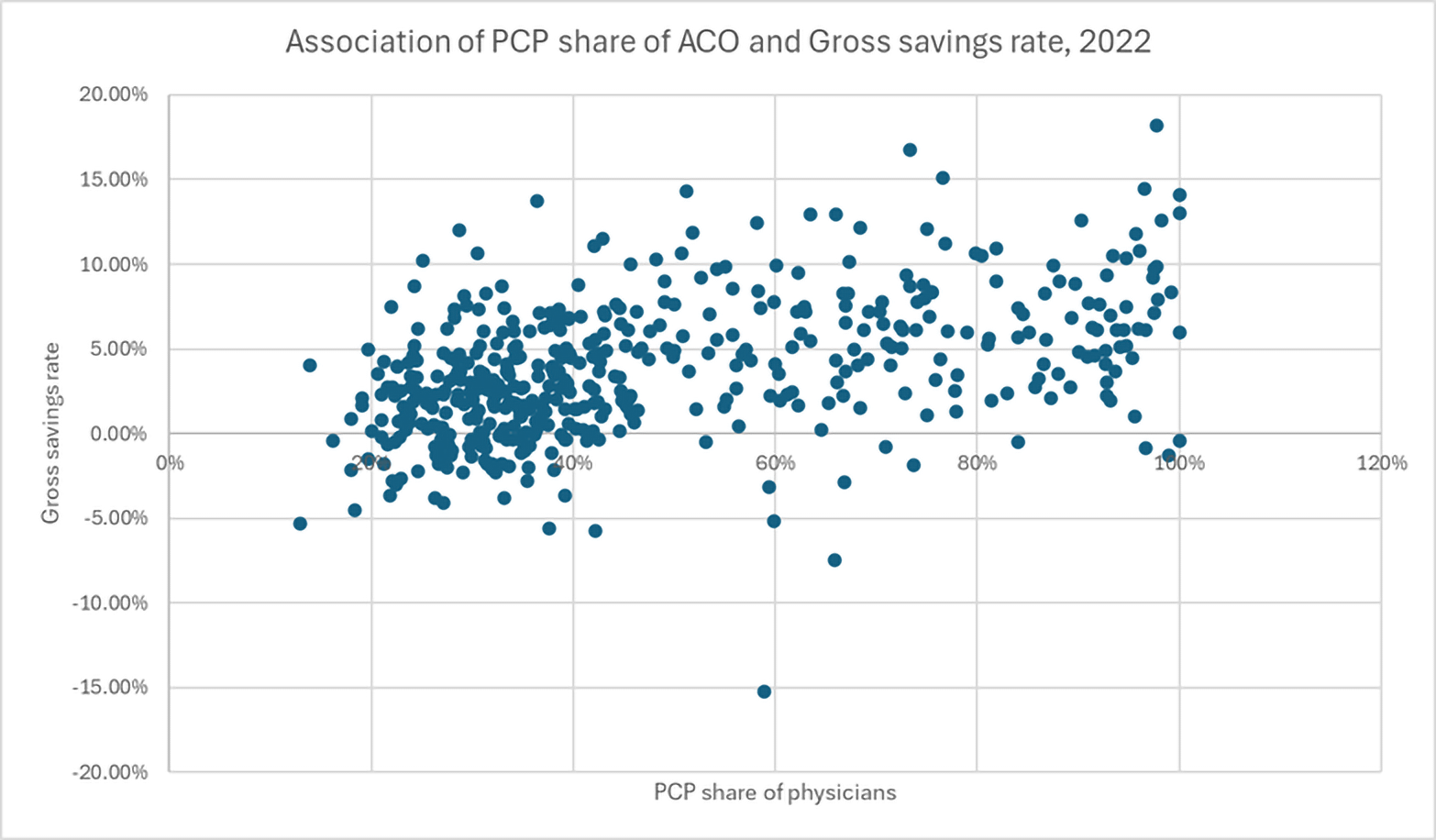
Less than half of all ACOs were physician-led in 2023,2 and the share of beneficiaries receiving care from physician-led ACOs has not been growing. Yet, analysis suggests ACOs predominantly comprised of primary care physicians (as a share of ACO physicians) are more likely to generate savings and higher savings than both hospital-led and physician-led ACOs with smaller shares of PCPs.
Why do “primary care-centric” ACOs outperform other ACOs?
Evidence suggests they do it by delivering more primary care to attributed beneficiaries, avoiding more preventable downstream costs (e.g., unnecessary hospital or ED visits) compared to other ACOs and keeping more care within the ACO.3
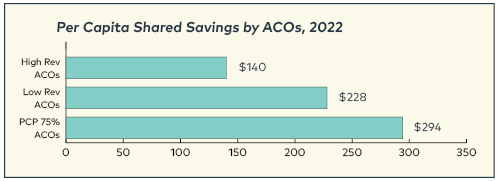
Analyses of both 20214 and 2022 MSSP results found, “more primary care physicians (PCPs) and more evaluation and management visits with PCPs lead to greater success.”5 The same analysis found “overwhelmingly that low revenue ACOs had greater levels of shared savings.“ When announcing MSSP results for 2022, CMS reported that ”low-revenue ACOs comprised of 75 percent primary care clinicians or more saw $294 per capita in net savings, more than twice as much (as high-revenue ACOs).”6
Encourage Primary Care Participation in Medicare ACOs
CMS should encourage more participation of primary care physicians and clinicians in Medicare ACOs and encourage ACOs to shift the composition of participating providers to primary care. Hospital-based ACOs should be strongly encouraged to refocus their efforts on supporting access to high-quality, comprehensive primary care. CMS should also foster engagement of primary care clinical leadership in ACO governance and decisions on resource allocation and development of tools and strategies to improve care and create more care access points.
Offer Primary Care Practices Optional Hybrid (FFS + PBPM) Payment in MSSP
- To attract more primary care professionals to join or form Medicare ACOs, CMS should offer an optional hybrid primary care payment to MSSP ACOs. Making all ACOs eligible for hybrid primary care payment could enable existing ACOs to improve performance and total cost-of-care savings.
- With upfront payment in the form of a per-beneficiary per-month (PBPM) amount, primary care practices can plan, build, and organize the teams and tech to deliver proactive care and improve the performance of ACOs. Simulations suggest the share of PBPM to FFS should be at least 60:40 to incentivize care transformation.7 This breakdown is similar to the Primary Care First model tested by CMMI. The PBPM amount should be adjusted for patient clinical and social risk and geography.
- CMS should use primary care utilization levels of the highest-performing primary care-centric ACOs with respect to how the hybrid payment level is set.
- Beneficiary cost-sharing should be waived for all services performed under the PBPM, and practices should have discretion to waive cost-sharing for in-person visits billed under the fee schedule.
- Because primary care-centric ACOs generate savings in the total cost of Part A and B by delivering more primary care,8 primary care-centric ACOs should not be expected to contribute to savings by reducing primary care expenditures or utilization. Rather, primary care should be expected and resourced, through a hybrid payment, to expand primary care access points and capacity, leveraging robust teams and technology.
1 Researchers have defined “physician-led” in different ways. In 2018, CMS created a distinction between “low” and “high” revenue ACOs defined by the share of total Part A and B spending for attributed beneficiaries was generated inside the ACO. High-revenue ACOs were defined as having more than 35% of annual total Part A & B spending of attributed beneficiaries. Low-revenue ACOs generally correspond to physician-led ACOs, and high-revenue ACOs correspond to hospital-led ACOs.
2 “Shared Savings Program Fast Facts - As of January 1, 2023.” Centers for Medicare and Medicaid Services. https://bit.ly/MSSPFastFacts
3 Lin, Sunny C., et al. “Out of Network Primary Care is Associated...” Health Affairs. February, 2020. https://bit.ly/Medicare-ACO-Spending
4 “Wakely Risk Insight for the Medicare Shared Savings Program: Performance Year 2021 Results.” Wakely Brief. October, 2022. https://bit.ly/Success-in-MSSP
5 “Wakely Risk Insight for the Medicare Shared Savings Program: Performance Year 2022 Results.” Wakely Brief. November, 2023. https://bit.ly/Wakely-MSSP-2022
6 “Medicare Shared Savings Program Saves Medicare More Than $1.8 Billion...” Centers for Medicare and Medicaid Services August, 2023. https://bit.ly/CMS-Savings-23
7 “High Levels Of Capitation Payments Needed To Shift Primary Care...” Health Affairs. September, 2017. https://bit.ly/PC-Value-Shift-HA
8 “Wakely Risk Insight for the Medicare Shared Savings Program: Performance Year 2022 Results.” Analysis found ACOs that deliver more E&M visits with primary care physicians correlates with higher gross savings.
| Attachment | Size |
|---|---|
| 290.31 KB |
Secondary menu
Copyright © 2024 Primary Care Collaborative



