You are looking at an archived version of our site. Please visit thepcc.org for a fresh, new experience!
You are here: Array » Primary Care & COV ...
Primary Care & COVID-19: Week 8 Survey
Check back weekly for the latest survey results and updates.
For last week's data, see Week 7 Results.
Who replied to the survey in Week 8?
Over 750 primary care clinicians responded to the survey in week 8. All states (with the exception of North Dakota) and Washington, D.C., participated. The largest share of the sample came from Virginia (12%), Texas (9%) and Oregon (7%), with Colorado, Rhode Island, and Washington each representing 5%. A new demographic question on practice size showed that 60% of the respondents work in a practice setting with fewer than 10 clinicians. Nearly a quarter work in rural practices, 18% at a community health center, and 9% at a convenience care setting. Over half (58%) serve greater than 10% Medicaid beneficiaries. The clinical specialty of respondents remained largely consistent with past weeks: 70% family medicine; 11% internal medicine; 7% pediatrics; 6% geriatrics; and 7% other.
Responses to week 8 of the survey were collected May 1-4, 2020. Total responses: 773.
Results at a glance
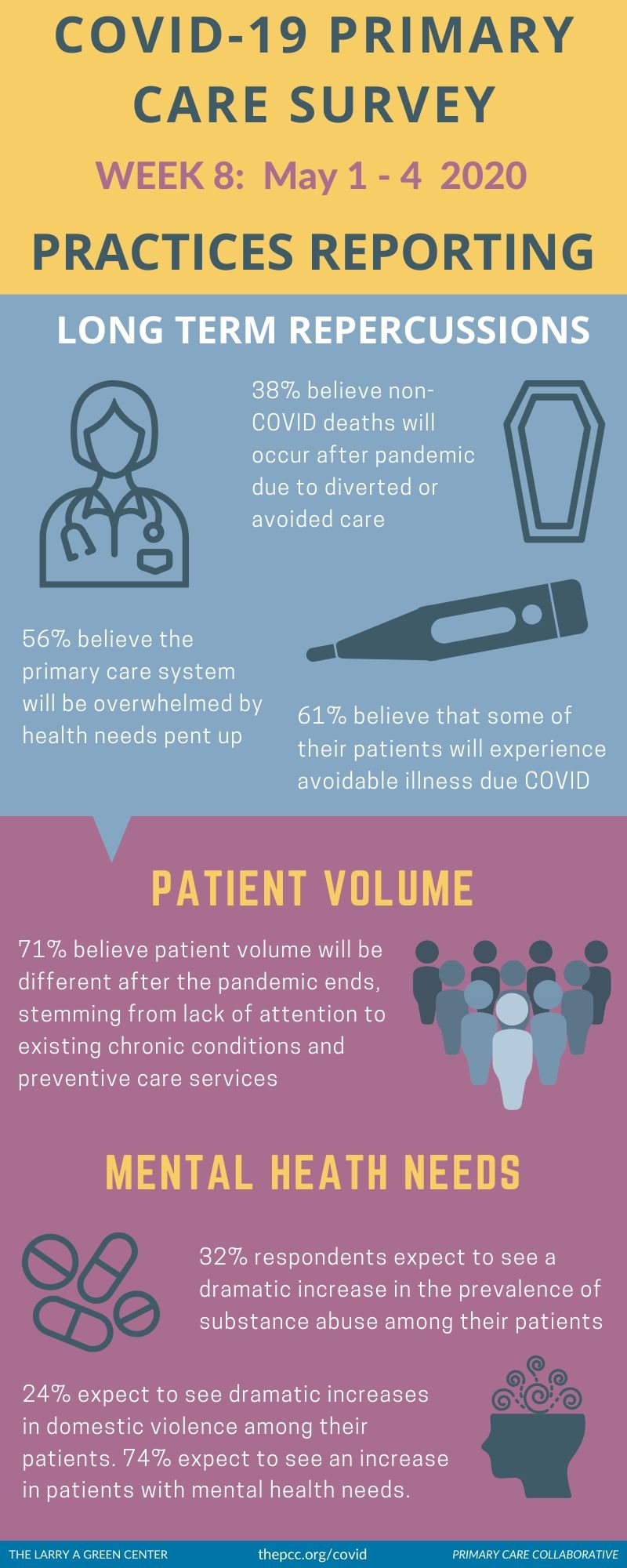
Clinicians believe that delayed care due to COVID-19 will mean serious—and sometimes fatal—repercussions for patients in the long-term. Thirty-eight percent of respondents believe that there will be non-COVID-19 related deaths among their patients after the pandemic ends due to diverted or avoided care; and over 60% believe that some of their patients will experience avoidable illness due to diverted or avoided care.
Concern for patients’ mental health needs, both now and post-pandemic, is mounting. Just under a third of respondents expect to see a dramatic increase in the prevalence of substance abuse among their patients; another quarter expect to see dramatic increases in domestic violence among their patients. 74% expect to see an increase in patients with mental health needs.
Clinicians fear that patients’ trust in the health care system is eroding. Clinicians’ own trust may be eroding too. A quarter of respondents say that they anticipate the pandemic will result in “a broken sense of trust between the public and the medical world”. Clinicians may be losing trust in the system too: 60% of respondents believe that policies changed to support primary care during COVID-19 will be reversed once the pandemic lessens.
A new primary care landscape—one with few independent practices—may emerge post-pandemic. Survey results highlight fears among primary care clinicians of a near-complete market consolidation stemming from the financial repercussions of the coronavirus. Over a third of respondents (35%) believe that the majority of independent primary care practices will be gone by the time the pandemic ends.
Primary care continues to call for a better public health response, but is skeptical it will come. With practices still lacking PPE (54%) and full testing capabilities (54%), nearly a third of respondents believe that the U.S. population and/or government has “accepted the unacceptable.” A full two-thirds say that the country will be opened too early, increasing the harms of the predicted second wave of COVID-19.
Slight financial improvements may be emerging. This week, 49% of clinicians report that over half of their visits were reimbursable (compared with 34% in week 7 and 43% in week 6). Still, 70% of respondents say they continue to see their patient volume down by more than half compared to before the pandemic.
Learn more: Download the Green Center/Primary Care Collaborative’s Executive Summary, which includes select open-ended answers to survey questions.
Voices from the Primary Care Front Lines
Corrosive "new normal" leaves many clinicians feeling abandoned and unheard.
No one cares. We are alone. I feel like giving up. I care so much for my patients but how long can I keep this up? (Delaware)
I worry every day that I will lose my practice. I am becoming depressed and losing hope with each passing day. (Washington)
I feel like I was hung out to dry. Take chances with my health or abandon my patients were my only choices since I could not get PPE. Our billers are on lockdown in India so nothing has been billed for months. (New York)
It has been the most stressful time of my 20-year career. Trying to care for pts with high-quality care, provide safe environment for our staff and maintaining a financially viable practice. Very much considering leaving clinical medicine. (Colorado)
Financial support recently made available is not reliably reaching practices in need.
Being owned by a hospital system, all the aid goes to the hospital not the physicians. My hospital keeps the CARES Act bonus and I still get a pay cut. THERE IS NOTHING FOR EMPLOYED PHYSICIANS. WE ARE IN FINANCIAL DISTRESS AND NOBODY IS ADDRESSING THIS. PAID 100% ON PRODUCTION AND I’M SEEING 30-40% OF USUAL VOLUME. WE NEED HELP. (Tennessee)
My office is small, 5 employees including myself. I have had to lay-off 2. My practice was first opened in January. We saw a 40% hit in our reimbursement for March/April. Stimulus money is based on last year’s tax returns, so no help for us. (Washington)
PPP loans are incredibly slow to come through and might not arrive in time to cover April payroll needs. (Texas)
Virtual health expanded rapidly as a patch fix, but some challenges are beginning to show.
For the short-term, it has been helpful. For the long-term, it makes us feel distant and dis-connected. Patients are increasingly isolated, depressed, anxious. Many choose to come in even though we could address their concerns virtually. (Oregon)
I actually love it - I’m a geriatrician and some patients w/ dementia and dementia-related behaviors are incredibly stressed when they have to be brought to clinic - video and telephone visits have actually improved their stress in that regard. (Illinois)
…insurers making it more difficult - codes change and 10 flavors of how to code telemedicine so I get paid for my work - ridiculous. We have no help. (Washington)
It has been more difficult to connect to 'underserved' patients with limited ability to manage virtual care. These relationships are stressed, and trust may erode if we cannot adapt to better serve them. (Michigan)
Increased capacity to identify medication-related problems as most patients contacted are home with their medication vials and glucometer or home blood pressure monitor, as applicable. (Illinois)
| Fichier attaché | Taille |
|---|---|
| 143.01 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
September 30, 2021 | Primary Care Collaborative
September 10, 2021 | MedPage Today
August 23, 2021 | STAT
August 19, 2021 | WalletHub
August 18, 2021 | Urban Institute
- ‹ précédent
- 5 of 39
- suivant ›
Recent News
August 16, 2024
August 12, 2024
July 16, 2024
RT @LarryMcNeely1: Here are the details for Making Care Primary program https://t.co/Uzkcipspsh —
Il y a 2 années 8 mois
RT @LarryMcNeely1: Critically, the model has 3 tracks, including new investments for practices in tracks 1 and 2! —
Il y a 2 années 8 mois
RT @LarryMcNeely1: Primary Care First practices volunteered to report data....but MORE practices need access to a)hybrid payment and better… —
Il y a 2 années 8 mois
Secondary menu
Copyright © 2024 Primary Care Collaborative