You are looking at an archived version of our site. Please visit thepcc.org for a fresh, new experience!
You are here: Array » Primary Care & COV ...
Primary Care & COVID-19: Week 5 Survey
Check back weekly for the latest survey results and updates.
For last week's data, see Week 4 Results.
Who replied to the survey in Week 5?
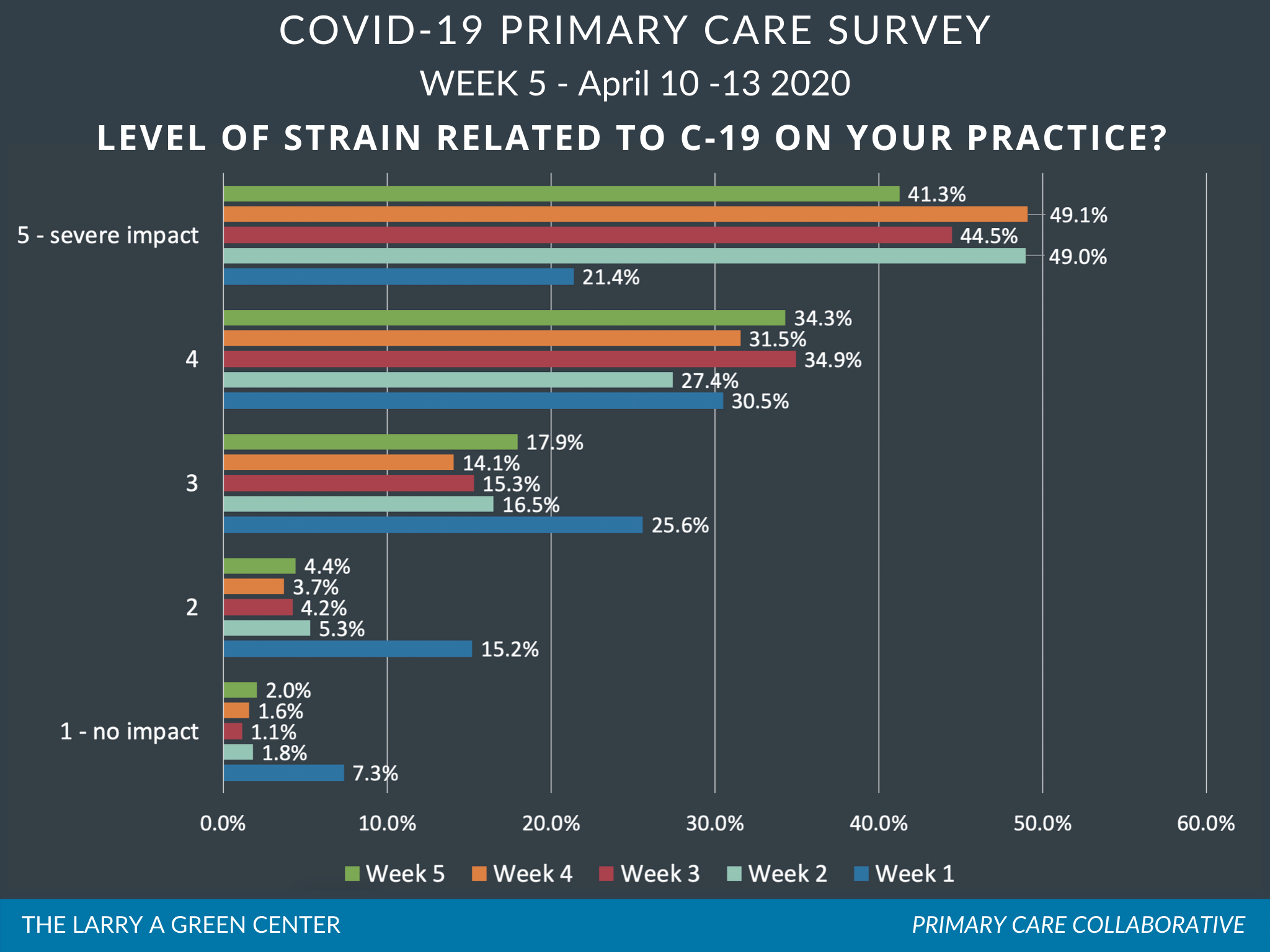
Week 5 received the highest number of responses yet: Over 2,600 primary care clinicians responded to the survey that was open April 10-13.
Responses spanned all 50 states, Washington, D.C., and key territories. The leading three states were Virginia (10% of total responses), Washington state (7%), and Texas (6%). Other states with 100 or more responses included California, Pennsylvania, Indiana, and Florida. Family medicine continued to be the dominant specialty among respondents (69%), followed by internal medicine (12%), geriatrics (7%), pediatrics (5%), urgent care (3%), and other (4%). Just under a third of respondents worked at practices with three or fewer clinicians. Compared to previous weeks, fewer respondents work in practices that they either own themselves (14%) or are owned by an academic medical center (13%). This week’s respondents were more likely to work in a rural setting (33%) and more likely to have more than half of their patients on Medicaid (37%). Twenty-seven percent work in a community health center.
Results at a glance
Patients are affected differently by COVID-19 based on their age, income, and race/ethnicity. 12% of surveyed clinicians see disparities among racial minorities; 27% among low income patients; 20% among those lacking computer/internet access; 29% among those with mental health conditions; and 33% among the elderly.
COVID-19 is taking a personal toll on both patients and health care professionals. Two-thirds of respondents report “rising family and economic concerns among patients” as a stress on their practice; 60% report similar family and income concerns among practice members.
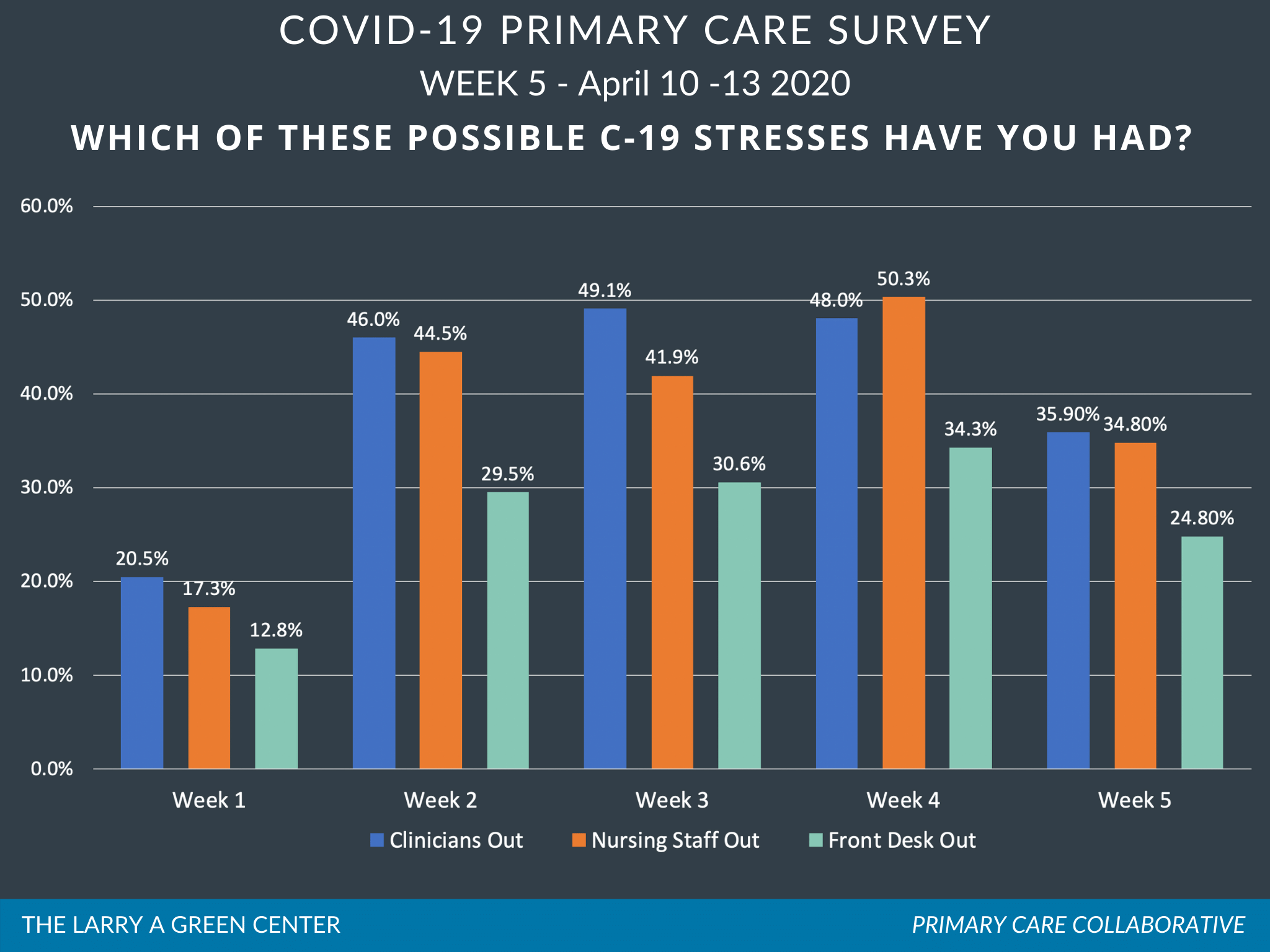
Financial strain on primary care practices is impacting their ability to keep staff employed and doors open. 42% of respondents report the “need to layoff or furlough practice members” as a stress on their practice. Fewer than half of respondents feel they had enough patient volume to stay open for the next four weeks (46%) or enough cash on-hand to stay open for the next four weeks (47%).
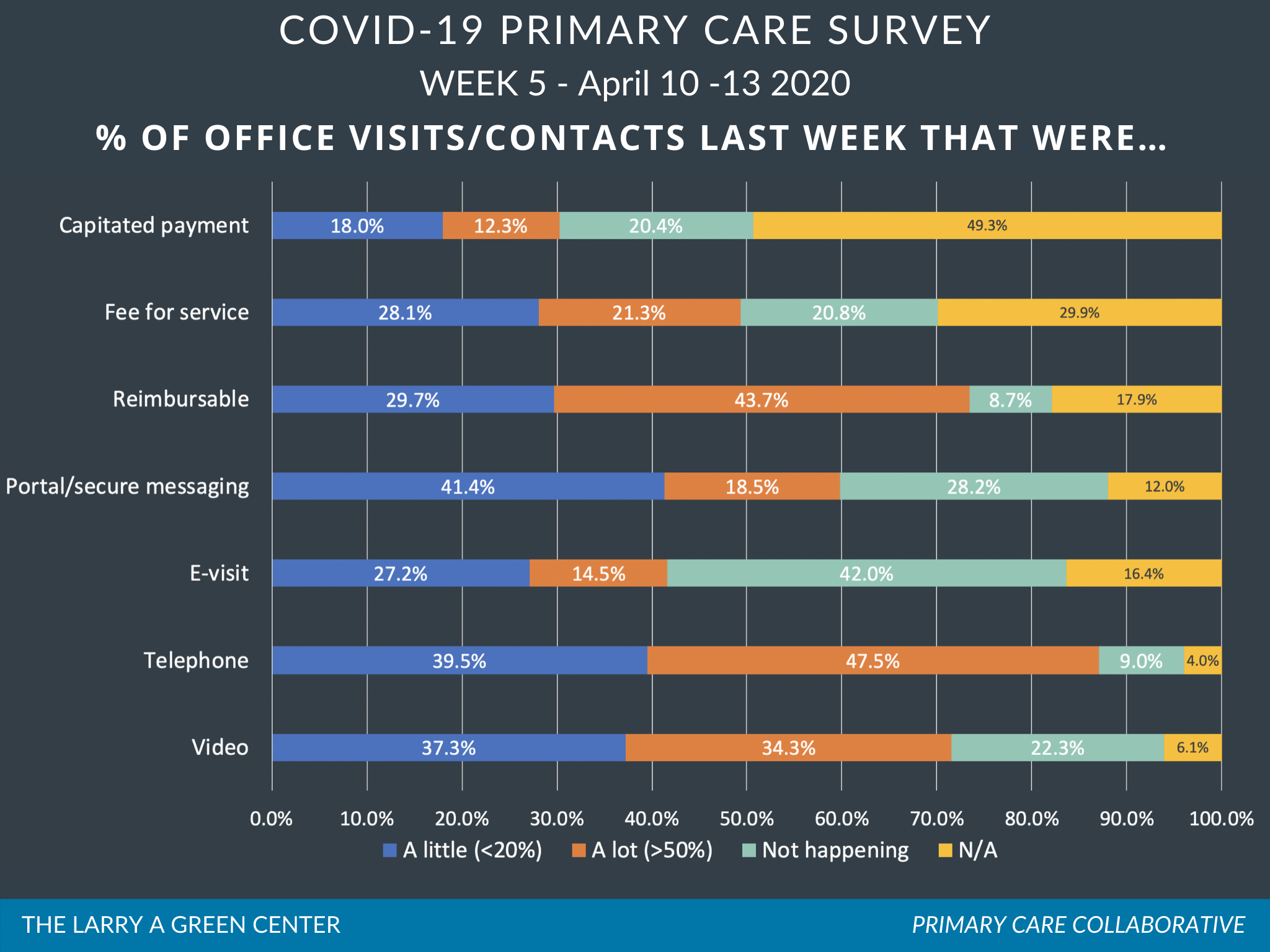
External financial support is increasing, but may be slow to arrive. Just under a fifth of respondents say that their practice is likely to apply for a Small Business Administration loan in the next four weeks. And the majority of respondents are uncertain that they will receive payments for virtual care: “likely to receive payment for video and e-based care?” No: 10%; 43%: Unsure; “likely to receive payment for your telephone-based care?” No: 16%; 44%: Unsure.
Learn more: Download the Green Center’s Executive Summary, which includes select open-ended answers to survey questions.
Voices from the Primary Care Front Lines
70% of clinicians reported trends in reasons for COVID-19-related health disparities and burdens
Low income and minority patients are harder to reach by phone because they are working. At our clinic, Latinx patients make up 80% of positive results but 40% of tests. (CA)
Patients with addictions hurt greatly. (WI)
I live near a reservation, they are more affected as they live in multigenerational houses, and have no running water. (NM)
Wage earners are feeling very stressed. And those with mental health issues are breaking through what used to be effective doses of medications - they are not coping well. (PA)
Fear is high among Chinese and SE Asian patients. People who need to work are at risk and have no PPE from employers. (OR)
54% of clinicians are focused on continued stress related to finances, testing availability and accuracy, and PPE. For example:
I voluntarily closed my practice weeks ago except for virtual visits due to the risk of exposure for my patients, I continue to pay my staff out of pocket but have reduced hours and am not receiving any income myself. (SC)
HELP! WE NEED HELP! I WORK ALL HOURS AND I'M MAKING NOTHING! I used one of my precious few tests of myself. I have COVID-19. I no longer see patients in person but I still do telehealth or they have no one. (VA)
Emergency loans (EIDL/PPP) are not processing nearly as quickly as promised, making cash flow concerns even more dire. (TX)
I am concerned about sustainability of unaffiliated primary care practices. We have such limited resources to begin with, then told we are too far down the list to get needed supplies like gloves, PPE and testing kits to do our jobs. (OR)
I am a Family Practice MD w/ 30 years experience who has just filed for unemployment for the first time in my life. (VA)
23% of clinicians focused on payment and access, frustrations with telehealth, and policy-driven obstacles to care
I have a large Medicare population. Many do not have video options. Please please talk to government about getting reimbursed same as audiovisual with telephone visits. Desperate... (VA)
Allow my pharmacists to be included in all of the billing and reimbursement. They are filling the gap in care. Do not discount payment due to telehealth. We are all still spending the same time with patients--it is not cheaper delivery!!! (IL)
Televisits are happened but we are not getting paid for them, there needs to be a single standard across insurers rather than having a patchwork of complicated requirements designed to not pay us for our work. (NH)
21% of respondents discussed primary care clinicians employed within systems suffering greater lack of autonomy and greater risk
We were initially told not to wear masks as it would frighten the patients. Then a nurse tested positive. (AZ)
We are owned by a hospital. They were VERY aggressive preparing the hospital for COVID but initially gave virtually no attention to the outpatient setting and how to manage patients with minimal symptoms who are nevertheless contagious to staff. (VA)
| Fichier attaché | Taille |
|---|---|
| 804.02 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- suivant ›

Recent News
August 16, 2024
August 12, 2024
July 16, 2024
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
Il y a 2 années 8 mois
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
Il y a 2 années 8 mois
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
Il y a 2 années 8 mois
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative